Assistant Professor Jaime Ross and her lab report surprising findings on the impact of short-term microplastics exposure through drinking water.
August 4, 2023
When Jaime Ross set out to investigate the impact of microplastics on human health as we age, she wasn’t expecting what she found.
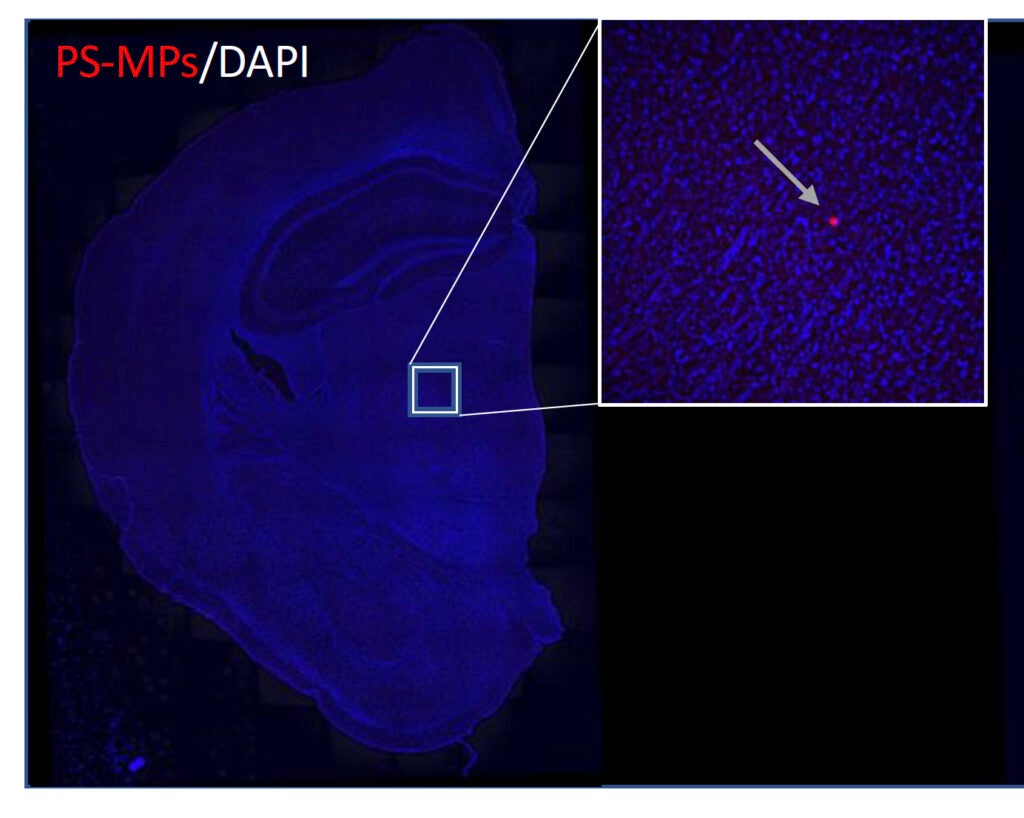
In a new study, Ross, an assistant professor of biomedical and pharmaceutical sciences at the Ryan Institute for Neuroscience, looked into effects of short-term exposure to microplastics—minute plastic particles—in young and old mice. Her lab not only found that the particles induced cognitive changes, but they were also able to cross the highly protective brain blood barrier.
“We were very surprised to see that,” said Ross. “The brain blood barrier is supposed to be very difficult to permeate. It is a protective mechanism against viruses and bacteria, yet these particles were able to get there. It was actually deep in the brain tissue.”
Microplastics, which form from the breakdown of larger plastics and also are used to create many commercial products, are a source of environmental pollution that are known to affect oceans and marine life. However, little is known about how the particles affect humans—or how much humans are being exposed to microplastics through their drinking water, consumption of seafood or plants, or the use of cosmetics and other products.
As part of URI’s Plastics: Land to Sea collaboration, Ross brings her longtime focus on aging and brain health to questions around the health impact of microplastics exposure. Her research team includes Research Assistant Professor Giuseppe Coppotelli, biomedical and pharmaceutical sciences graduate student Lauren Gaspar, who is first author on the paper, and INP graduate student Sydney Bartman.
“Nobody really understands the life cycle of these microplastics in the body, so part of what we want to address is the question of what happens as you get older,” says Ross. “Are you more susceptible to systemic inflammation from these microplastics as you age? Can your body get rid of them as easily? Do your cells respond differently to these toxins? We also really want to understand if there are differences in how males and females respond to the toxins.”
In the recent study, the Ross lab found that in just three weeks of exposure to microplastics through drinking water, the particles had not only begun to bioaccumulate in every organ, including the brain, but also that the study mice exhibited behaviors akin to dementia in humans.
“To us, this was striking,” says Ross. “These were not high doses of microplastics, but in only a short period of time, we saw these changes.”
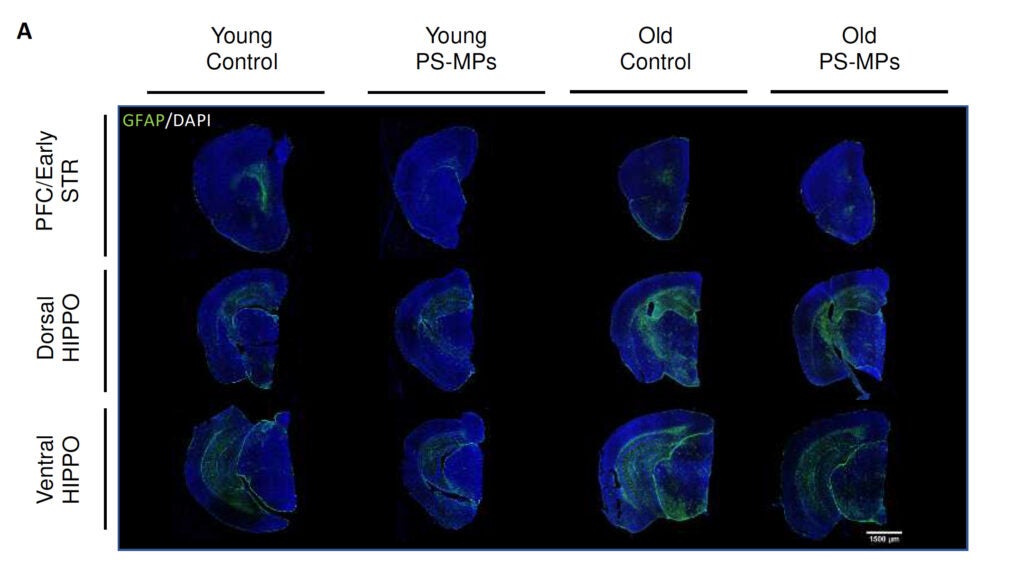
She adds that while the lab expected to see some amount of inflammation in response to the microplastics exposure, they also found a decrease in glial fibrillary acidic protein (called “GFAP”), a protein that supports many cell processes in the brain. “A decrease in GFAP has been associated with early stages of some neurodegenerative diseases, including mouse models of Alzheimer’s disease, as well as depression,” says Ross. “We were very surprised to see that the microplastics could induce altered GFAP signaling.”
She intends to investigate this finding further in future work. “We want to understand how plastics may change the ability for the brain to maintain its homeostastis or how exposure may lead to neurological disorders and diseases, such as Alzheimer’s disease,” she says.
The study was published in the International Journal of Molecular Science. It was supported by the Rhode Island Medical Research Foundation, the Roddy Foundation, the Plastics Initiative, the College of Pharmacy, and the George and Anne Ryan Institute for Neuroscience at URI, as well as by the Rhode Island Institutional Development Award (IDeA) Network of Biomedical Research Excellence from the National Institute of General Medical Sciences of the National Institutes of Health.