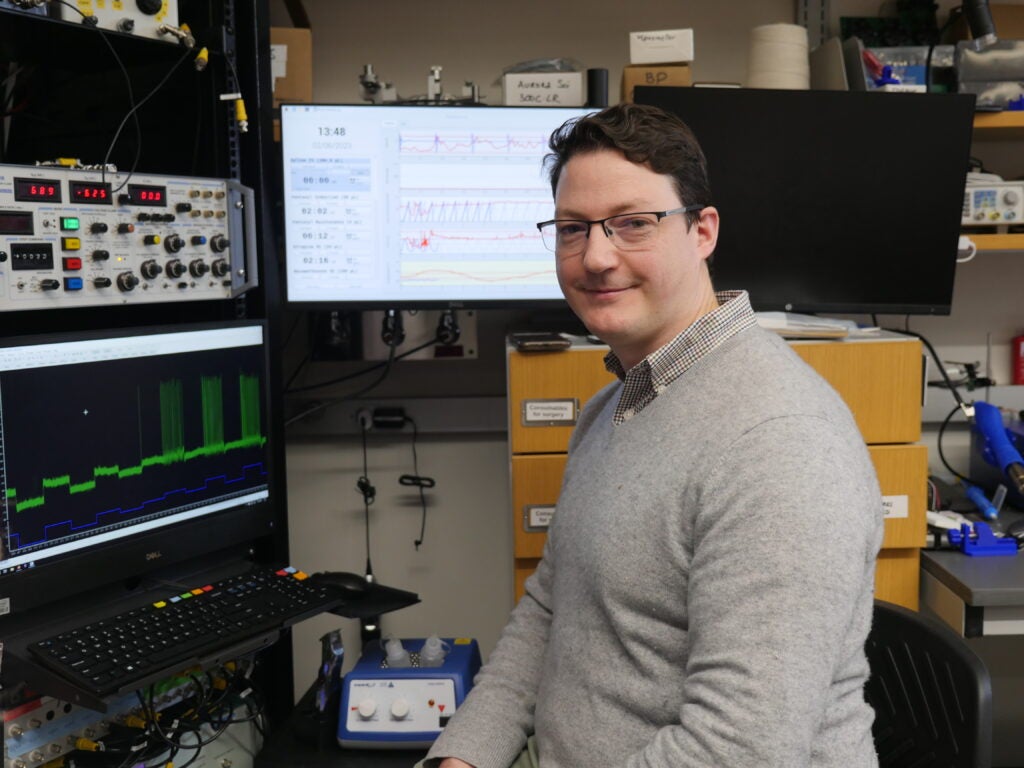
Using his unique in vivo approach, Assistant Professor Marin Manuel investigates electrical activity in the spinal motor neurons in a disease model of amyotrophic lateral sclerosis.
Also known as Lou Gehrig’s disease, amyotrophic lateral sclerosis (ALS) is a mysterious and fatal disorder where nerve cells in the brain and spinal cord break down, rapidly progressing from the first symptoms of muscle weakness to the complete loss of muscle control and function. Researchers don’t yet know what causes the disease, but Marin Manuel, assistant professor of biomedical and pharmaceutical sciences, is focused on a potential clue: In ALS, motor neurons deteriorate and die, but not all once.
Manuel wondered if the differences between faster-dying neurons and those that deteriorate more slowly could provide a key to understanding which motor neurons are most vulnerable to the disease. However, to investigate this question, he first needed to identify motor neuron subtypes, something that hadn’t been done before.
“I was interested in the fact that there are a lot of different types of neurons involved in different tasks,” says Manuel. “I wanted to understand how they acquire different identities and properties.”
Using electrophysiology, his lab developed a unique in vivo approach to record the electrical activity of neurons in a mouse model spinal cord simultaneously with muscle output, allowing him to observe which motor neuron subtypes control which muscles.
“Once we could identify the different subtypes of motor neurons, it was a big step toward trying to figure out what electrical changes might be important or related to the degeneration process,” says Manuel.
With subtypes identified, he compared electrical activity in a normal mouse model to the activity in a disease model—and found something unexpected. While existing research done in brain cells supports that motor neurons in ALS go into a hyperactive state before they essentially “burn out” and die, Manuel’s work in the spinal cord neurons indicates the opposite.
“It seems to us that a decrease in the level of activity of neurons is detrimental to their survival,” says Manuel. “When they fail to function, they degenerate.”
His lab has discovered that restoring the electrical activity in failing neurons significantly slows the degeneration process. “We still don’t know what causes the initial decrease in activity, but we’ve shown that if we force the motor neurons to respond more, they survive longer,” he says.
He hopes that these findings could point to a way to extend the time that motor neurons remain functional in ALS.
“ALS is a very fast-progressing disease,” says Manuel. “Most people survive only three or five years after diagnosis. Anything we can do to slow it down could help patients stay mobile and independent for a longer period of time.”
Manuel is also encouraged by the possibilities for novel recording techniques in further investigations of ALS. “We’ve obtained very promising preliminary recordings from hundreds of recording sites in the mouse spinal cord,” he says. “It’s a brand new development in the field of neuroscience, and I hope that it can lead to us knowing much more about the mechanisms of this disease.”