BRAIN HEALTH • JUNE 2018
The Inflammation Connection
W. Sue T. Griffin, Ph.D. was a young researcher when she identified a surprising similarity between the cells in the immune system and in the brain. Thirty-five years later, she has helped transform what we know about neuroinflammation–and what we can do to prevent it.
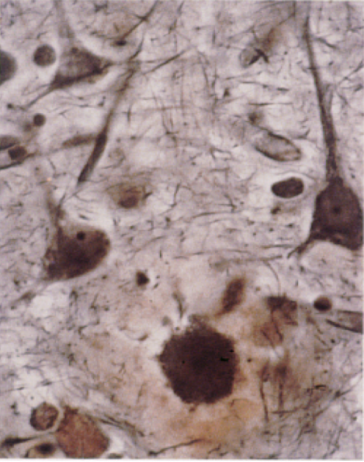
SUE GRIFFIN REMEMBERS the lightbulb moment. She was attending a lecture on Alzheimer’s disease, looking at projections of silver-stained slides of dying neurons, and noting how the surrounding microglia and astrocytes (two types of cells found in the brain) were enlarged like macrophages—white blood cells in the immune system that eat up harmful debris and microbes. While scientists at the time knew microglia in the brain could mimic the behavior of macrophages, immune responses in the brain were still mostly undiscovered. As she looked at the amyloid plaques on the slides, littered like trash bags among the cells, it occurred to her: If microglia could act like macrophages, did they also produce the same inflammatory proteins?
At the end of the seminar, Griffin turned to the friend seated beside her. “‘I think I know what is happening in Alzheimer’s,’” she recalls saying. “‘And if I’m right, aspirin will cure it.’”
More on aspirin later. In the past thirty-five years since that seminar, Griffin’s research has helped to pioneer the field of neuroinflammation and our understanding of the brain’s immune responses in neurodegenerative disease. In 1989, she published a ground-breaking paper on interleukin-1 (IL-1) in Alzheimer’s, identifying it as playing an integral role in the development of the disease. Just as macrophages in the immune system could become overly stressed to produce a destructive cycle of chronic inflammation, Griffin’s research found a similar cycle happening in the Alzheimer’s brain, where IL-1—a small protein that plays a beneficial role in acute inflammation but that is linked to joint deterioration in arthritis—helps drive the progression of Alzheimer’s, triggering the formation of amyloid plaques and tau tangles (both hallmarks of the disease) and the deterioration of brain cells.
This May, Griffin visited the Ryan Institute, where she is a member of the scientific advisory board, to discuss her work.
Some highlights from her talk:
• “A little inflammation is okay,” said Griffin. “Chronic, no way.” While inflammation is the body’s way of protecting itself from harm, chronic inflammation contributes to a number of disorders and diseases. Lifestyle choices—such as keeping blood sugar, blood pressure, and cholesterol at healthy levels—can play a significant role in preventing the chronic inflammation that causes disease. Today, there is widespread and increasing research to support the role of a heart-healthy lifestyle in preventing Alzheimer’s.
• To cut disease-causing inflammation, exercise and eat your vegetables. “You’ve got to eat all colors of fruits, vegetables, and spices,” Griffin said. “Obesity and type-2 diabetes increases your risk of Alzheimer’s almost as much as having the Alzheimer’s gene,” said Griffin, referring to the ApoE4 gene linked to the development of early-onset Alzheimer’s. In Rhode Island, 27% of Rhode Islanders are obese (up 17% since 2000)*, the same percentage at risk for Alzheimer’s, she noted. Exercise is beneficial not only in keeping weight at a healthy level but in reducing stress and inflammation.
• Protect your head. Head injuries can have a lasting impact in causing stress to the brain and damaging neuro-inflammation.
• “A merry heart doeth good like a medicine” is one of Griffin’s favorite quotes. Keeping the mind active, through learning and hobbies, and staying socially connected are important to long-term brain health. “It’s never too late,” said Griffin, on the chance to make a positive change in your physical and mental health.
And what about aspirin? While Alzheimer’s is a complex disease, with multiple factors likely playing a role in its development and progression, the role of inflammation in the disease has made aspirin and ibuprofen an ongoing area of research interest. “Look for it,” Griffin says. “Aspirin is going to be a part of it.
See the video of the talk here.
– Nicole Maranhas
Biography
Sue T. Griffin, Ph.D. is the Alexa and William T. Dillard Professor and Vice Chairman of Research at the Donald W. Reynolds Department of Geriatrics at University of Arkansas for Medical Sciences, and the director of basic research for the Donald W. Reynolds Institute on Aging. In 2016, she received the 2016 Alzheimer’s Association Lifetime Achievement Award for her contributions to neurodegenerative disease research. She is editor-in-chief of the Journal of Neuroinflammation.
*Statistics from the Centers for Disease Control